
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Enhancing Patient Outcomes: Prioritizing SGLT2is and GLP-1RAs in Diabetes with CVD
- Gwanpyo Koh
- Diabetes Metab J. 2024;48(2):208-212. Published online March 22, 2024
- DOI: https://doi.org/10.4093/dmj.2024.0096
- 683 View
- 108 Download
- Metabolic Risk/Epidemiology
- Current Status of Low-Density Lipoprotein Cholesterol Target Achievement in Patients with Type 2 Diabetes Mellitus in Korea Compared with Recent Guidelines
- Soo Jin Yun, In-Kyung Jeong, Jin-Hye Cha, Juneyoung Lee, Ho Chan Cho, Sung Hee Choi, SungWan Chun, Hyun Jeong Jeon, Ho-Cheol Kang, Sang Soo Kim, Seung-Hyun Ko, Gwanpyo Koh, Su Kyoung Kwon, Jae Hyuk Lee, Min Kyong Moon, Junghyun Noh, Cheol-Young Park, Sungrae Kim
- Diabetes Metab J. 2022;46(3):464-475. Published online March 3, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0088
- 6,937 View
- 347 Download
- 4 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
We evaluated the achievement of low-density lipoprotein cholesterol (LDL-C) targets in patients with type 2 diabetes mellitus (T2DM) according to up-to-date Korean Diabetes Association (KDA), European Society of Cardiology (ESC)/European Atherosclerosis Society (EAS), and American Diabetes Association (ADA) guidelines.
Methods
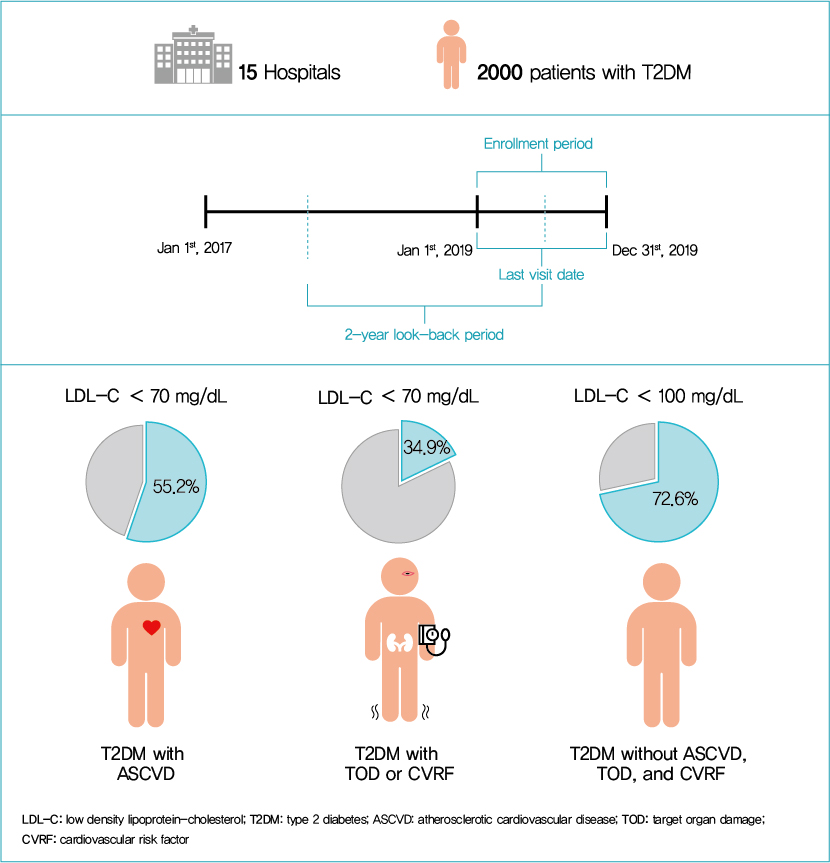
This retrospective cohort study collected electronic medical record data from patients with T2DM (≥20 years) managed by endocrinologists from 15 hospitals in Korea (January to December 2019). Patients were categorized according to guidelines to assess LDL-C target achievement. KDA (2019): Very High-I (atherosclerotic cardiovascular disease [ASCVD]) <70 mg/dL; Very High-II (target organ damage [TOD], or cardiovascular risk factors [CVRFs]) <70 mg/dL; high (others) <100 mg/dL. ESC/EAS (2019): Very High-I (ASCVD): <55 mg/dL; Very High-II (TOD or ≥3-CVRF) <55 mg/dL; high (diabetes ≥10 years without TOD plus any CVRF) <70 mg/dL; moderate (diabetes <10 years without CVRF) <100 mg/dL. ADA (2019): Very High-I (ASCVD); Very High-II (age ≥40+ TOD, or any CVRF), for high intensity statin or statin combined with ezetimibe.
Results
Among 2,000 T2DM patients (mean age 62.6 years; male 55.9%; mean glycosylated hemoglobin 7.2%) ASCVD prevalence was 24.7%. Of 1,455 (72.8%) patients treated with statins, 73.9% received monotherapy. According to KDA guidelines, LDL-C target achievement rates were 55.2% in Very High-I and 34.9% in Very High-II patients. With ESC/EAS guidelines, target attainment rates were 26.6% in Very High-I, 15.7% in Very High-II, and 25.9% in high risk patients. Based on ADA guidelines, most patients (78.9%) were very-high risk; however, only 15.5% received high-intensity statin or combination therapy.
Conclusion
According to current dyslipidemia management guidelines, LDL-C goal achievement remains suboptimal in Korean patients with T2DM. -
Citations
Citations to this article as recorded by- Risk factor control and cardiovascular events in patients with type 2 diabetes mellitus
Do Kyeong Song, Young Sun Hong, Yeon-Ah Sung, Hyejin Lee, Hidetaka Hamasaki
PLOS ONE.2024; 19(2): e0299035. CrossRef - Distinct effects of rosuvastatin and rosuvastatin/ezetimibe on senescence markers of CD8+ T cells in patients with type 2 diabetes mellitus: a randomized controlled trial
Sang-Hyeon Ju, Joung Youl Lim, Minchul Song, Ji Min Kim, Yea Eun Kang, Hyon-Seung Yi, Kyong Hye Joung, Ju Hee Lee, Hyun Jin Kim, Bon Jeong Ku
Frontiers in Endocrinology.2024;[Epub] CrossRef - Lipid Management in Korean People With Type 2 Diabetes Mellitus: Korean Diabetes Association and Korean Society of Lipid and Atherosclerosis Consensus Statement
Ye Seul Yang, Hack-Lyoung Kim, Sang-Hyun Kim, Min Kyong Moon
Journal of Lipid and Atherosclerosis.2023; 12(1): 12. CrossRef - Lipid Management in Korean People with Type 2 Diabetes Mellitus: Korean Diabetes Association and Korean Society of Lipid and Atherosclerosis Consensus Statement
Ye Seul Yang, Hack-Lyoung Kim, Sang-Hyun Kim, Min Kyong Moon
Diabetes & Metabolism Journal.2023; 47(1): 1. CrossRef - Management of Dyslipidemia in Patients with Diabetes Mellitus
Kyung Ae Lee
The Journal of Korean Diabetes.2023; 24(3): 111. CrossRef - Association between carotid atherosclerosis and presence of intracranial atherosclerosis using three-dimensional high-resolution vessel wall magnetic resonance imaging in asymptomatic patients with type 2 diabetes
Ji Eun Jun, You-Cheol Hwang, Kyu Jeong Ahn, Ho Yeon Chung, Geon-Ho Jahng, Soonchan Park, In-Kyung Jeong, Chang-Woo Ryu
Diabetes Research and Clinical Practice.2022; 191: 110067. CrossRef
- Risk factor control and cardiovascular events in patients with type 2 diabetes mellitus
- Clinical Diabetes & Therapeutics
- Effectiveness and Safety of Adding Basal Insulin Glargine in Patients with Type 2 Diabetes Mellitus Exhibiting Inadequate Response to Metformin and DPP-4 Inhibitors with or without Sulfonylurea
- Yu Mi Kang, Chang Hee Jung, Seung-Hwan Lee, Sang-Wook Kim, Kee-Ho Song, Sin Gon Kim, Jae Hyeon Kim, Young Min Cho, Tae Sun Park, Bon Jeong Ku, Gwanpyo Koh, Dol Mi Kim, Byung-Wan Lee, Joong-Yeol Park
- Diabetes Metab J. 2019;43(4):432-446. Published online June 19, 2019
- DOI: https://doi.org/10.4093/dmj.2018.0092
- 5,554 View
- 89 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background We aimed to investigate the effectiveness and safety of adding basal insulin to initiating dipeptidyl peptidase-4 (DPP-4) inhibitor and metformin and/or sulfonylurea (SU) in achieving the target glycosylated hemoglobin (HbA1c) in patients with type 2 diabetes mellitus (T2DM).
Methods This was a single-arm, multicenter, 24-week, open-label, phase 4 study in patients with inadequately controlled (HbA1c ≥7.5%) T2DM despite the use of DPP-4 inhibitor and metformin. A total of 108 patients received insulin glargine while continuing oral antidiabetic drugs (OADs). The primary efficacy endpoint was the percentage of subjects achieving HbA1c ≤7.0%. Other glycemic profiles were also evaluated, and the safety endpoints were adverse events (AEs) and hypoglycemia.
Results The median HbA1c at baseline (8.9%; range, 7.5% to 11.1%) decreased to 7.6% (5.5% to 11.7%) at 24 weeks. Overall, 31.7% subjects (
n =33) achieved the target HbA1c level of ≤7.0%. The mean differences in body weight and fasting plasma glucose were 1.2±3.4 kg and 56.0±49.8 mg/dL, respectively. Hypoglycemia was reported in 36 subjects (33.3%, 112 episodes), all of which were fully recovered. There was no serious AE attributed to insulin glargine. Body weight change was significantly different between SU users and nonusers (1.5±2.5 kg vs. −0.9±6.0 kg,P =0.011).Conclusion The combination add-on therapy of insulin glargine, on metformin and DPP-4 inhibitors with or without SU was safe and efficient in reducing HbA1c levels and thus, is a preferable option in managing T2DM patients exhibiting dysglycemia despite the use of OADs.
-
Citations
Citations to this article as recorded by- Glycaemic control with add‐on thiazolidinedione or a sodium‐glucose co‐transporter‐2 inhibitor in patients with type 2 diabetes after the failure of an oral triple antidiabetic regimen: A 24‐week, randomized controlled trial
Jaehyun Bae, Ji Hye Huh, Minyoung Lee, Yong‐Ho Lee, Byung‐Wan Lee
Diabetes, Obesity and Metabolism.2021; 23(2): 609. CrossRef - Beneficial effect of anti-diabetic drugs for nonalcoholic fatty liver disease
Kyung-Soo Kim, Byung-Wan Lee
Clinical and Molecular Hepatology.2020; 26(4): 430. CrossRef
- Glycaemic control with add‐on thiazolidinedione or a sodium‐glucose co‐transporter‐2 inhibitor in patients with type 2 diabetes after the failure of an oral triple antidiabetic regimen: A 24‐week, randomized controlled trial
- Pathophysiology
- Factors Related to Blood Intact Incretin Levels in Patients with Type 2 Diabetes Mellitus
- Soyeon Yoo, Eun-Jin Yang, Gwanpyo Koh
- Diabetes Metab J. 2019;43(4):495-503. Published online February 20, 2019
- DOI: https://doi.org/10.4093/dmj.2018.0105
- 3,918 View
- 36 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background We performed this study to identify factors related to intact incretin levels in patients with type 2 diabetes mellitus (T2DM).
Methods We cross-sectionally analyzed 336 patients with T2DM. Intact glucagon-like peptide 1 (iGLP-1) and intact glucose-dependent insulinotropic polypeptide (iGIP) levels were measured in a fasted state and 30 minutes after ingestion of a standard mixed meal. The differences between 30 and 0 minute iGLP-1 and iGIP levels were indicated as ΔiGLP-1 and ΔiGIP.
Results In simple correlation analyses, fasting iGLP-1 was positively correlated with glucose, C-peptide, creatinine, and triglyceride levels, and negatively correlated with estimated glomerular filtration rate. ΔiGLP-1 was positively correlated only with ΔC-peptide levels. Fasting iGIP showed positive correlations with glycosylated hemoglobin (HbA1c) and fasting glucose levels, and negative correlations with ΔC-peptide levels. ΔiGIP was negatively correlated with diabetes duration and HbA1c levels, and positively correlated with Δglucose and ΔC-peptide levels. In multivariate analyses adjusting for age, sex, and covariates, fasting iGLP-1 levels were significantly related to fasting glucose levels, ΔiGLP-1 levels were positively related to ΔC-peptide levels, fasting iGIP levels were related to fasting C-peptide levels, and ΔiGIP levels were positively related to ΔC-peptide and Δglucose levels.
Conclusion Taken together, intact incretin levels are primarily related to C-peptide and glucose levels. This result suggests that glycemia and insulin secretion are the main factors associated with intact incretin levels in T2DM patients.
- Changes in Adenosine Deaminase Activity in Patients with Type 2 Diabetes Mellitus and Effect of DPP-4 Inhibitor Treatment on ADA Activity
- Jae-Geun Lee, Dong Gu Kang, Jung Re Yu, Youngree Kim, Jinsoek Kim, Gwanpyo Koh, Daeho Lee
- Diabetes Metab J. 2011;35(2):149-158. Published online April 30, 2011
- DOI: https://doi.org/10.4093/dmj.2011.35.2.149
- 4,201 View
- 33 Download
- 28 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Dipeptidyl peptidase 4 (DPP-4, also known as CD26) binds with adenosine deaminase (ADA) to activate T lymphocytes. Here, we investigated whether ADA activity is specifically affected by treatment with DPP-4 inhibitor (DPP4I) compared with other anti-diabetic agents.
Methods Fasting ADA activity, in addition to various metabolic and biochemical parameters, were measured in 262 type 2 diabetes mellitus (T2DM) patients taking various anti-diabetic agents and in 46 non-diabetic control subjects.
Results ADA activity was increased in T2DM patients compared with that in non-diabetic control subjects (mean±standard error, 23.1±0.6 U/L vs. 18.6±0.8 U/L;
P <0.05). ADA activity was correlated with fasting plasma glucose (r =0.258,P <0.05), HbA1c (r =0.208,P <0.05), aspartate aminotransferase (r =0.325,P <0.05), and alanine aminotransferase (r =0.248,P <0.05). Compared with the well-controlled T2DM patients (HbA1c<7%), the poorly controlled group (HbA1c>9%) showed significantly increased ADA activity (21.1±0.8 U/L vs. 25.4±1.6 U/L;P <0.05). The effect of DPP4I on ADA activity in T2DM patients did not differ from those of other oral anti-diabetic agents or insulin. T2DM patients on metformin monotherapy showed a lower ADA activity (20.9±1.0 U/L vs. 28.1±2.8 U/L;P <0.05) compared with that of those on sulfonylurea monotherapy.Conclusion Our results show that ADA activity is increased in T2DM patients compared to that in non-diabetic patients, is positively correlated with blood glucose level, and that DPP4I has no additional specific effect on ADA activity, except for a glycemic control- or HbA1c-dependent effect.
-
Citations
Citations to this article as recorded by- Influence of BMI on adenosine deaminase and stroke outcomes in mechanical thrombectomy subjects
Benton Maglinger, Christopher J. McLouth, Jacqueline A. Frank, Chintan Rupareliya, Madison Sands, Lila Sheikhi, Shivani Pahwa, David Dornbos, Jordan P. Harp, Amanda L. Trout, Jadwiga Turchan-Cholewo, Ann M. Stowe, Justin F. Fraser, Keith R. Pennypacker
Brain, Behavior, & Immunity - Health.2022; 20: 100422. CrossRef - Glutamine restores testicular glutathione-dependent antioxidant defense and upregulates NO/cGMP signaling in sleep deprivation-induced reproductive dysfunction in rats
M.A. Hamed, T.M. Akhigbe, R.E. Akhigbe, A.O. Aremu, P.A. Oyedokun, J.A. Gbadamosi, P.E. Anifowose, M.A. Adewole, O.O. Aboyeji, H.O. Yisau, G.O. Tajudeen, M.M. Titiloye, N.F. Ayinla, A.F. Ajayi
Biomedicine & Pharmacotherapy.2022; 148: 112765. CrossRef - Effects of quercetin and metabolites on uric acid biosynthesis and consequences for gene expression in the endothelium
Sarka Tumova, Yuanlu Shi, Ian M. Carr, Gary Williamson
Free Radical Biology and Medicine.2021; 162: 191. CrossRef - The value of adenosine deaminase activity in latent autoimmune diabetes in adults and type 2 diabetes patients
Yu Zhou, Wei-Dong Jin, Zhen-Zhen Pang, Jun Xia, Su-Feng Chen
International Journal of Diabetes in Developing Countries.2021; 41(1): 48. CrossRef - Purinergic signaling in diabetes and metabolism
Shanu Jain, Kenneth A. Jacobson
Biochemical Pharmacology.2021; 187: 114393. CrossRef - Berberine modulates crucial erectogenic biomolecules and alters histological architecture in penile tissues of diabetic rats
Stephen Adeniyi Adefegha, Ganiyu Oboh, Felix Abayomi Dada, Sunday Idowu Oyeleye, Bathlomew Maduka Okeke
Andrologia.2021;[Epub] CrossRef - Suppression of uric acid and lactate production by sodium acetate ameliorates hepatic triglyceride accumulation in fructose-insulin resistant pregnant rats
Adewumi O. Oyabambi, Kehinde S. Olaniyi, Ayodele O. Soladoye, Lawrence A. Olatunji
Environmental Toxicology and Pharmacology.2020; 80: 103452. CrossRef - Therapeutic Perspectives of Adenosine Deaminase Inhibition in Cardiovascular Diseases
Barbara Kutryb-Zajac, Paulina Mierzejewska, Ewa M. Slominska, Ryszard T. Smolenski
Molecules.2020; 25(20): 4652. CrossRef - Adenosine as a Marker and Mediator of Cardiovascular Homeostasis: A Translational Perspective
Trevor Simard, Richard Jung, Alisha Labinaz, Mohammad Ali Faraz, F. Daniel Ramirez, Pietro Di Santo, Ian Pitcher, Pouya Motazedian, Chantal Gaudet, Rebecca Rochman, Jeffrey Marbach, Paul Boland, Kiran Sarathy, Saleh Alghofaili, Juan J. Russo, Etienne Cout
Cardiovascular & Hematological Disorders-Drug Targets.2019; 19(2): 109. CrossRef - Mineralocorticoid receptor blockade attenuates disrupted glutathione-dependent antioxidant defense and elevated endoglin in the hearts of pregnant rats exposed to testosterone
Taofeek O. Usman, Olufunto O. Badmus, InKyeom Kim, Lawrence A. Olatunji
Naunyn-Schmiedeberg's Archives of Pharmacology.2019; 392(7): 773. CrossRef - Serum activities of dipeptidyl peptidase-4 and adenosine deaminase in polycystic ovary syndrome: association with obesity
Seda Kahraman, Alev Eroglu Altinova, Serenay Elgun, Mehmet Muhittin Yalcin, Banu Aktas Yilmaz, Cigdem Ozkan, Mujde Akturk, Fusun Balos Toruner
Gynecological Endocrinology.2019; 35(8): 714. CrossRef - Serum adenosine deaminase activity and coronary artery disease: a retrospective case-control study based on 9929 participants
Chao Xuan, Qing-Wu Tian, Shao-Yan Zhang, Hui Li, Ting-Ting Tian, Peng Zhao, Kang Yue, Yan-Yan Ling, Guo-Wei He, Li-Min Lun
Therapeutic Advances in Chronic Disease.2019; 10: 204062231989153. CrossRef - Metabolites related to purine catabolism and risk of type 2 diabetes incidence; modifying effects of the TCF7L2-rs7903146 polymorphism
Christopher Papandreou, Jun Li, Liming Liang, Mònica Bulló, Yan Zheng, Miguel Ruiz-Canela, Edward Yu, Marta Guasch-Ferré, Cristina Razquin, Clary Clish, Dolores Corella, Ramon Estruch, Emilio Ros, Montserrat Fitó, Fernando Arós, Lluís Serra-Majem, Nuria R
Scientific Reports.2019;[Epub] CrossRef - Current status of G-protein coupled receptors as potential targets against type 2 diabetes mellitus
Mehboob Hoque, Safdar Ali, Muddasarul Hoda
International Journal of Biological Macromolecules.2018; 118: 2237. CrossRef - Endoglin inhibition by sodium acetate and flutamide ameliorates cardiac defective G6PD-dependent antioxidant defense in gestational testosterone-exposed rats
Lawrence A. Olatunji, Emmanuel D. Areola, Olufunto O. Badmus
Biomedicine & Pharmacotherapy.2018; 107: 1641. CrossRef - Sodium acetate and androgen receptor blockade improve gestational androgen excess-induced deteriorated glucose homeostasis and antioxidant defenses in rats: roles of adenosine deaminase and xanthine oxidase activities
Taofeek O. Usman, Emmanuel D. Areola, Olufunto O. Badmus, InKyeom Kim, Lawrence A. Olatunji
The Journal of Nutritional Biochemistry.2018; 62: 65. CrossRef - ADENOSINE DEAMINASE ACTIVITY IN TYPE 2 DIABETES MELLITUS
Farija Peruvankuzhiyil, Lavanya Madhavan, Manaloor George Joseraj
Journal of Evidence Based Medicine and Healthcare.2017; 4(5): 238. CrossRef - Adenosine signaling in diabetes mellitus and associated cardiovascular and renal complications
Maria Peleli, Mattias Carlstrom
Molecular Aspects of Medicine.2017; 55: 62. CrossRef - The Adenosinergic System in Diabetic Retinopathy
J. Vindeirinho, A. R. Santiago, C. Cavadas, A. F. Ambrósio, P. F. Santos
Journal of Diabetes Research.2016; 2016: 1. CrossRef - Upregulation of inducible NO synthase by exogenous adenosine in vascular smooth muscle cells activated by inflammatory stimuli in experimental diabetes
Alberto Nassi, Francesca Malorgio, Serena Tedesco, Andrea Cignarella, Rosa Maria Gaion
Cardiovascular Diabetology.2016;[Epub] CrossRef - Reduced adenosine A2a receptor–mediated efferent arteriolar vasodilation contributes to diabetes-induced glomerular hyperfiltration
Patrik Persson, Peter Hansell, Fredrik Palm
Kidney International.2015; 87(1): 109. CrossRef - CD26/DPP4 Levels in Peripheral Blood and T Cells in Patients With Type 2 Diabetes Mellitus
Sang Ah Lee, Young Ree Kim, Eun Jin Yang, Eun-Jeong Kwon, Sun Hyung Kim, Sung Ha Kang, Doek Bae Park, Byung-Chul Oh, Jinseok Kim, Sang Taek Heo, Gwanpyo Koh, Dae Ho Lee
The Journal of Clinical Endocrinology & Metabolism.2013; 98(6): 2553. CrossRef - Raised Serum Adenosine Deaminase Level in Nonobese Type 2 Diabetes Mellitus
Vineet Kumar Khemka, Debajit Bagchi, Arindam Ghosh, Oishimaya Sen, Aritri Bir, Sasanka Chakrabarti, Anindita Banerjee
The Scientific World Journal.2013; 2013: 1. CrossRef - Phosphodiesterase III Inhibition Increases cAMP Levels and Augments the Infarct Size Limiting Effect of a DPP-4 Inhibitor in Mice with Type-2 Diabetes Mellitus
Yochai Birnbaum, Alexander C. Castillo, Jinqiao Qian, Shukuan Ling, Hongmei Ye, Jose R. Perez-Polo, Mandeep Bajaj, Yumei Ye
Cardiovascular Drugs and Therapy.2012; 26(6): 445. CrossRef - Serum Adenosine deaminase activity in type 2 Diabetes Mellitus patients
M. N. Vanitha Gowda, K. C. Vasudha, S. Reshma, K. J. Sujatha
International Journal of Diabetes in Developing Countries.2012; 32(3): 176. CrossRef - Cyclic AMP and PKA: How can a Lot of Good Come from the Potentially Bad?
Barbara Huisamen
Cardiovascular Drugs and Therapy.2012; 26(6): 435. CrossRef - Gadd45α: A Novel Diabetes-Associated Gene Potentially Linking Diabetic Cardiomyopathy and Baroreflex Dysfunction
Ning Wang, Chao Yang, Fang Xie, Lihua Sun, Xiaolin Su, Ying Wang, Ran Wei, Rong Zhang, Xia Li, Baofeng Yang, Jing Ai, Rajesh Gopalrao Katare
PLoS ONE.2012; 7(12): e49077. CrossRef - The CD39-Adenosinergic Axis in the Pathogenesis of Immune and Nonimmune Diabetes
Joanne S. J. Chia, Jennifer L. McRae, Peter J. Cowan, Karen M. Dwyer
Journal of Biomedicine and Biotechnology.2012; 2012: 1. CrossRef
- Influence of BMI on adenosine deaminase and stroke outcomes in mechanical thrombectomy subjects
- Clinical Characteristics of Type 2 Diabetes Patients according to Family History of Diabetes
- Seung Uk Jeong, Dong Gu Kang, Dae Ho Lee, Kang Woo Lee, Dong-Mee Lim, Byung Joon Kim, Keun-Yong Park, Hyoun-Jung Chin, Gwanpyo Koh
- Korean Diabetes J. 2010;34(4):222-228. Published online August 31, 2010
- DOI: https://doi.org/10.4093/kdj.2010.34.4.222
- 3,477 View
- 26 Download
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Type 2 diabetes mellitus (T2DM) has a strong genetic component, and its prevalence is notably increased in the family members of T2DM patients. However, there are few studies about the family history of T2DM. We carried out this study to assess the influences of family history on clinical characteristics in T2DM patients.
Methods This is a cross-sectional study involving 651 T2DM patients. Patient history and physical examination were performed and fasting blood was taken. If any first degree relative was diabetic, a family history of diabetes was considered to exist.
Results Among the total 621 patients, 38.4% had a family history of diabetes. Patients with a family history had a younger age, higher weight, younger age at diagnosis and higher triglyceride level than did those without a family history. Dyslipidemia medication and metabolic syndrome were more prevalent in familial diabetes. Sex, blood pressure, previous treatment for diabetes, HbA1c, C-peptide, total cholesterol, high density lipoprotein cholesterol, and low density lipoprotein cholesterol were not different between familial and non-familial diabetes. Upon multiple linear regression analysis, the family history of diabetes remained significantly associated with serum triglyceride level.
Conclusion In T2DM patients with a family history of diabetes, the disease tended to develop earlier. Metabolic syndrome and cardiovascular risk factors are more prevalent in familial T2DM than they were in non-familial T2DM. These results support the necessity of earlier screening for diabetes in family members of T2DM patients and more active prevention against cardiovascular disease in T2DM patients with a family history.
-
Citations
Citations to this article as recorded by- COVID-19-Induced Diabetes Mellitus: Comprehensive Cellular and Molecular Mechanistic Insights
Praise Tatenda Nhau, Mlindeli Gamede, Ntethelelo Sibiya
Pathophysiology.2024; 31(2): 197. CrossRef - Evolutionary algorithm for the optimization of meal intake and insulin administration in patients with type 2 diabetes
Eva Gonzalez-Flo, Elaheh Kheirabadi, Carlos Rodriguez-Caso, Javier Macía
Frontiers in Physiology.2023;[Epub] CrossRef - Role of Cytokines (IL-17 and IL-33), FGF-18, and WNT-5 in the Pathogenesis of Patients with Established Type II Diabetes
Przha Mohammed, Kawa Amin
Journal of Zankoy Sulaimani - Part A.2023; 25(2): 11. CrossRef - Cellular Chitchatting: Exploring the Role of Exosomes as Cardiovascular Risk Factors
Giulia Germena, Laura Cecilia Zelarayán, Rabea Hinkel
Frontiers in Cell and Developmental Biology.2022;[Epub] CrossRef - Combined associations of family history and self-management with age at diagnosis and cardiometabolic risk in 86,931 patients with type 2 diabetes: Joint Asia Diabetes Evaluation (JADE) Register from 11 countries
Johnny T. K. Cheung, Eric Lau, Cyrus C. T. Tsui, Edmond L. N. Siu, Naomi K. W. Tse, Nicole Y. L. Hui, Ronald C. W. Ma, Alice P. S. Kong, Amy Fu, Vanessa Lau, Weiping Jia, Wayne H. H. Sheu, Leorino Sobrepena, K. H. Yoon, Alexander T. B. Tan, Yook-Chin Chia
BMC Medicine.2022;[Epub] CrossRef - Capsaicin, its clinical significance in patients with painful diabetic neuropathy
Phiwayinkosi V. Dludla, Bongani B. Nkambule, Ilenia Cirilli, Fabio Marcheggiani, Sihle E. Mabhida, Khanyisani Ziqubu, Yonela Ntamo, Babalwa Jack, Tawanda M. Nyambuya, Sidney Hanser, Sithandiwe E. Mazibuko-Mbeje
Biomedicine & Pharmacotherapy.2022; 153: 113439. CrossRef - Safety profile of sodium glucose co-transporter 2 (SGLT2) inhibitors: A brief summary
Annamaria Mascolo, Raffaella Di Napoli, Nunzia Balzano, Donato Cappetta, Konrad Urbanek, Antonella De Angelis, Lucia Scisciola, Irene Di Meo, Maria Giuseppa Sullo, Concetta Rafaniello, Liberata Sportiello
Frontiers in Cardiovascular Medicine.2022;[Epub] CrossRef - Impact of triglycerides and waist circumference on insulin resistance and β-cell function in non-diabetic first-degree relatives of type 2 diabetes
Fahd Ahmed, Molham AL-Habori, Ebtesam Al-Zabedi, Riyadh Saif-Ali
BMC Endocrine Disorders.2021;[Epub] CrossRef - Orientin Improves Substrate Utilization and the Expression of Major Genes Involved in Insulin Signaling and Energy Regulation in Cultured Insulin-Resistant Liver Cells
Sithandiwe E. Mazibuko-Mbeje, Sinenhlanhla X. H. Mthembu, Andani Tshiitamune, Ndivhuwo Muvhulawa, Fikile T. Mthiyane, Khanyisani Ziqubu, Christo J. F. Muller, Phiwayinkosi V. Dludla
Molecules.2021; 26(20): 6154. CrossRef - Identification of Pre-Diabetic Biomarkers in the Progression of Diabetes Mellitus
Jae-Ho Lee, Do-Young Kim, Rubee Pantha, Eun-Ho Lee, Jae-Hoon Bae, Eugene Han, Dae-Kyu Song, Taeg Kyu Kwon, Seung-Soon Im
Biomedicines.2021; 10(1): 72. CrossRef - Shared (epi)genomic background connecting neurodegenerative diseases and type 2 diabetes
Valerio Caputo, Andrea Termine, Claudia Strafella, Emiliano Giardina, Raffaella Cascella
World Journal of Diabetes.2020; 11(5): 155. CrossRef - Family history of diabetes in both parents is strongly associated with impaired residual β‐cell function in Japanese type 2 diabetes patients
Minoru Iwata, Yutaka Kamura, Hisae Honoki, Kaori Kobayashi, Manabu Ishiki, Kunimasa Yagi, Yasuo Fukushima, Atsuko Takano, Hiromi Kato, Shihou Murakami, Kiyohiro Higuchi, Chikaaki Kobashi, Kazuhito Fukuda, Yukiko Koshimizu, Kazuyuki Tobe
Journal of Diabetes Investigation.2020; 11(3): 564. CrossRef - The relationship between age of onset and risk factors including family history and life style in Korean population with type 2 diabetes mellitus
Jin-Won Noh, Jin Hee Jung, Jeong Eun Park, Jung Hwa Lee, Kang Hee Sim, Jumin Park, Min Hee Kim, Ki-Bong Yoo
Journal of Physical Therapy Science.2018; 30(2): 201. CrossRef - Clinical Characteristics of Subjects with Sulfonylurea-Dependent Type 2 Diabetes
Se Hee Min, Soo Heon Kwak, Young Min Cho, Kyong Soo Park, Hye Seung Jung
Endocrinology and Metabolism.2015; 30(4): 509. CrossRef - Nutritional Assessment of Type II Diabetic Patients
El-Sayed H. Bakr
Pakistan Journal of Nutrition.2015; 14(6): 308. CrossRef
- COVID-19-Induced Diabetes Mellitus: Comprehensive Cellular and Molecular Mechanistic Insights
- Clinical Experience of the Reverse Iontophoresis Based Glucose Measuring System: Glucall(TM).
- Sang Youl Rhee, Suk Chon, Gwanpyo Koh, Seungjoon Oh, Jeong taek Woo, Sung Woon Kim, Jin Woo Kim, Young Seol Kim
- Korean Diabetes J. 2009;33(2):167-167. Published online April 1, 2009
- DOI: https://doi.org/10.4093/kdj.2009.33.2.167
- 1,717 View
- 22 Download
-
 Abstract
Abstract
 PDF
PDF - To the editor, My original paper that published in Journal of Korean Diabetes Association 2005;29:167-172, entitled, Clinical Experience of the Reverse Iontophoresis Based Glucose Measuring System: Glucall(TM) was submitted to other international journals by me and the coauthor at the same time independently. I hereby retract the paper.
- A Nationwide Survey about the Current Status of Glycemic Control and Complications in Diabetic Patients in 2006: The Committee of the Korean Diabetes Association on the Epidemiology of Diabetes Mellitus.
- Soo Lim, Dae Jung Kim, In Kyung Jeong, Hyun Shik Son, Choon Hee Chung, Gwanpyo Koh, Dae Ho Lee, Kyu Chang Won, Jeong Hyun Park, Tae Sun Park, Jihyun Ahn, Jaetaek Kim, Keun Gyu Park, Seung Hyun Ko, Yu Bae Ahn, Inkyu Lee
- Korean Diabetes J. 2009;33(1):48-57. Published online February 1, 2009
- DOI: https://doi.org/10.4093/kdj.2009.33.1.48
- 2,770 View
- 55 Download
- 43 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The Committee of the Korean Diabetes Association on the Epidemiology of Diabetes Mellitus performed a nationwide survey about the current status of glycemic control and diabetic complications in 2006. METHODS: The current study included 5,652 diabetic patients recruited from the rosters of endocrinology clinics of 13 tertiary hospitals in Korea. Age, gender, height, weight, waist circumference and blood pressure were investigated by standard method. Fasting and postprandial 2 hour glucose, glycosylated hemoglobin (HbA1c), lipid profiles, fasting insulin and c-peptide levels were measured. Microvascular (microalbuminuria, retinopathy and neuropathy) and macrovascular (coronary artery disease [CAD], cerebrovascular disease [CVD] and peripheral artery disease [PAD]) complications were reviewed in their medical records. RESULTS: Mean age of total subjects was 58.7 (+/- 11.6) years and duration of diabetes was 8.8 (0~50) years. Mean fasting and postprandial 2 hour glucose levels were 145.9 +/- 55.0 and 208.0 +/- 84.4 mg/dL, respectively. Their mean HbA1c was 7.9 +/- 1.9%: the percentage of patients within target goal of glycemic control (< 7% of HbA1c) was 36.7%. In this study, 30.3%, 38.3% and 44.6% of patients was found to have microalbuminuria, retinopathy and nephropathy, respectively. Prevalence of CAD, CVD and PAD was 8.7%, 6.7% and 3.0%, respectively. Diabetic complications were closely related with age, duration of diabetes and glycemic control, and this relationship was stronger in microvascular complications than macrovascular ones. CONCLUSION: Only about one third of patients with diabetes was found to reach target glycemic control in tertiary hospitals of Korea. More tight control is needed to reduce deleterious complications of diabetes in Korea. -
Citations
Citations to this article as recorded by- Risk of Diabetic Complications in Type 2 Diabetes Patients with Dementia: A Population-Based Study Using National Health Insurance Claims Data
Eun Sik Jeong, Ah-Young Kim, Hye-Young Kang
Drug Targets and Therapeutics.2023; 2(1): 49. CrossRef - Prevalence of thyroid disorders in type 2 diabetic patients – A 1-year cross-sectional study
RikitaRamesh Mudhol, ShivakumarVeeranna Turamari, RekhaRamesh Mudhol, B Srinivas
BLDE University Journal of Health Sciences.2022; 7(1): 56. CrossRef - Associations of fasting glucose and glycated hemoglobin with vitamin D levels according to diabetes mellitus status in Korean adults
Yerin Hwang, Jiyoung Jang, Myung-Hee Shin
Epidemiology and Health.2022; 44: e2022025. CrossRef - Atherectomy in Peripheral Artery Disease: Current and Future
Yohan Kwon, Jinoo Kim, Je-Hwan Won, Seong Ho Kim, Jeong-Eun Kim, Sung-Joon Park
Journal of the Korean Society of Radiology.2021; 82(3): 551. CrossRef - Diabetic Retinopathy and Related Clinical Practice for People with Diabetes in Korea: A 10-Year Trend Analysis
Yoo-Ri Chung, Kyoung Hwa Ha, Kihwang Lee, Dae Jung Kim
Diabetes & Metabolism Journal.2020; 44(6): 928. CrossRef - Current status of treatment of type 2 diabetes mellitus in Ningbo, China
Tianmeng Yang, Rongjiong Zheng, Qingmei Chen, Yushan Mao
Journal of Clinical Laboratory Analysis.2019;[Epub] CrossRef - Recently Uncontrolled Glycemia in Diabetic Patients Is Associated with the Severity of Intracranial Atherosclerosis
Nari Choi, Jeong-Yoon Lee, Jun-Sang Sunwoo, Hakjae Roh, Moo-Young Ahn, Sung-Tae Park, Kyung Bok Lee
Journal of Stroke and Cerebrovascular Diseases.2017; 26(11): 2615. CrossRef - The effect of educational program based on the precede-proceed model on improving self-care behaviors in a semi-urban population with type 2 diabetes referred to health centers of Bavi, Iran
Neda Barasheh, Ghodratollah Shakerinejad, Sedigheh Nouhjah, Mohammad Hossein Haghighizadeh
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2017; 11: S759. CrossRef - Increased prevalence of albuminuria in individuals with higher range of impaired fasting glucose: the 2011 Korea National Health and Nutrition Examination Survey
Jong Chul Won, Jae Won Hong, Jung Min Kim, Tae Nyun Kim, Jung Hyun Noh, Kyung Soo Ko, Byoung Doo Rhee, Dong-Jun Kim
Journal of Diabetes and its Complications.2015; 29(1): 50. CrossRef - Assessment of glycemic control in patients with type 2 diabetes mellitus treated with metformin–sulfonylurea combination: Results of a multicenter, cross‐sectional, observational study in Korea
Sin Gon Kim, Jong Ryeal Hahm, Duk Kyu Kim, Sung Rae Cho, Dong Seop Choi
Journal of Diabetes Investigation.2015; 6(3): 317. CrossRef - Current Status of Management in Type 2 Diabetes Mellitus at General Hospitals in South Korea
Jin-Hee Jung, Jung-Hwa Lee, Jin-Won Noh, Jeong-Eun Park, Hee-Sook Kim, Joo-Wha Yoo, Bok-Rye Song, Jeong-rim Lee, Myeong-Hee Hong, Hyang-Mi Jang, Young Na, Hyun-Joo Lee, Jeong-Mi Lee, Yang-Gyo Kang, Sun-Young Kim, Kang-Hee Sim
Diabetes & Metabolism Journal.2015; 39(4): 307. CrossRef - Kidney injury molecule-1 (Kim-1): an early biomarker for nephropathy in type II diabetic patients
Nahla E. El-Ashmawy, Enas A. El-Zamarany, Naglaa F. Khedr, Abeer I. Abd El-Fattah, Shereen A. Eltoukhy
International Journal of Diabetes in Developing Countries.2015; 35(S3): 431. CrossRef - The Effect of the Experience of Diabetes Education on Knowledge, Self-Care Behavior and Glycosylated Hemoglobin in Type 2 Diabetic Patients
Seung Hei Moon, Young Whee Lee, Ok-Kyung Ham, Soo-Hyun Kim
The Journal of Korean Academic Society of Nursing Education.2014; 20(1): 81. CrossRef - Clinical Characteristics of Diabetic Patients Transferred to Korean Referral Hospitals
Min Young Oh, Sang Soo Kim, In Joo Kim, In Kyu Lee, Hong Sun Baek, Hyoung Woo Lee, Min Young Chung
Diabetes & Metabolism Journal.2014; 38(5): 388. CrossRef - Current Status of Prescription in Type 2 Diabetic Patients from General Hospitals in Busan
Ji Hye Suk, Chang Won Lee, Sung Pyo Son, Min Cheol Kim, Jun Hyeob Ahn, Kwang Jae Lee, Ja Young Park, Sun Hye Shin, Min Jeong Kwon, Sang Soo Kim, Bo Hyun Kim, Soon Hee Lee, Jeong Hyun Park, In Joo Kim
Diabetes & Metabolism Journal.2014; 38(3): 230. CrossRef - The Influence of Admission Hypoglycemia on Clinical Outcomes in Acute Myocardial Infarction Patients with Diabetes Mellitus
Eun Jung Kim, Myung Ho Jeong, In Seok Jeong, Sang Gi Oh, Sang Hyung Kim, Young keun Ahn, Ju Han Kim, Young Jo Kim, Shung Chull Chae, Taek Jong Hong, In Whan Seong, Jei Keon Chae, Chong Jin Kim, Myeong Chan Cho, Ki Bae Seung, Hyo Soo Kim
Korean Journal of Medicine.2014; 87(5): 565. CrossRef - Duration of diabetes and effectiveness of insulin in the management of insulin-naïve Korean patients uncontrolled on oral antidiabetic drugs: a sub-analysis of the MOdaliTy of Insulin treatment eValuation (MOTIV) registry results
Sang Soo Kim, In Joo Kim, Yong Ki Kim, Kun Ho Yoon, Ho Young Son, Sung Woo Park, Yeon Ah Sung, Hong Sun Baek, Kyoung Soo Ha
Acta Diabetologica.2014; 51(4): 655. CrossRef - Is the Indicator Magnifying Window for Insulin Pens Helpful for Elderly Diabetic Patients?
Ju Hee Lee, Eun Shil Hong, Jung Hun Ohn, Young Min Cho
Diabetes & Metabolism Journal.2013; 37(2): 149. CrossRef - Prevalence of and Factors Associated with Albuminuria in the Korean Adult Population: The 2011 Korea National Health and Nutrition Examination Survey
Jong Chul Won, Yun Jeong Lee, Jung Min Kim, Sang Youb Han, Jung Hyun Noh, Kyung Soo Ko, Byoung Doo Rhee, Dong-Jun Kim, Harald Mischak
PLoS ONE.2013; 8(12): e83273. CrossRef - The Epidemiology of Diabetic Nephropathy
Jin Hwa Kim
The Journal of Korean Diabetes.2013; 14(1): 11. CrossRef - The Relationship between Neuropathic Pain and Glycemic Control, Self Management in Type II Diabetes Mellitus Patients
Yeong-Mi Seo, Won-Hee Choi
Journal of the Korea Academia-Industrial cooperation Society.2013; 14(4): 1774. CrossRef - Efficacy and Safety of Biphasic Insulin Aspart 30/70 in Type 2 Diabetes Suboptimally Controlled on Oral Antidiabetic Therapy in Korea: A Multicenter, Open-Label, Single-Arm Study
Kee-Ho Song, Jung Min Kim, Jung-Hyun Noh, Yongsoo Park, Hyun-Shik Son, Kyong Wan Min, Kyung Soo Ko
Diabetes & Metabolism Journal.2013; 37(2): 117. CrossRef - Comorbidity Study on Type 2 Diabetes Mellitus Using Data Mining
Hye Soon Kim, A Mi Shin, Mi Kyung Kim, Yoon Nyun Kim
The Korean Journal of Internal Medicine.2012; 27(2): 197. CrossRef - Low ankle-brachial index is an independent predictor of poor functional outcome in acute cerebral infarction
Jinkwon Kim, Dong Hyun Lee, Myoung-Jin Cha, Tae-Jin Song, Ji Hye Park, Hye Sun Lee, Chung Mo Nam, Hyo Suk Nam, Young Dae Kim, Ji Hoe Heo
Atherosclerosis.2012; 224(1): 113. CrossRef - Glucose, Blood Pressure, and Lipid Control in Korean Adults with Diagnosed Diabetes
Sun-Joo Boo
Korean Journal of Adult Nursing.2012; 24(4): 406. CrossRef - Diabetic Peripheral Neuropathy in Type 2 Diabetes Mellitus in Korea
Seung-Hyun Ko, Bong-Yun Cha
Diabetes & Metabolism Journal.2012; 36(1): 6. CrossRef - The Association of Self-Reported Coronary Heart Disease with Diabetes Duration in Korea
Hye Mi Kang, Yun Jeong Lee, Dong-Jun Kim
Diabetes & Metabolism Journal.2012; 36(5): 350. CrossRef - Response: The Prevalence of Peripheral Arterial Disease in Korean Patients with Type 2 Diabetes Mellitus Attending a University Hospital (Diabetes Metab J 2011;35:543-50)
Ji Hee Yu, Ki-Up Lee
Diabetes & Metabolism Journal.2012; 36(1): 77. CrossRef - Reduction in glycated albumin can predict change in HbA1c: comparison of oral hypoglycaemic agent and insulin treatments
H. K. Won, K. J. Kim, B.‐W. Lee, E. S. Kang, B. S. Cha, H. C. Lee
Diabetic Medicine.2012; 29(1): 74. CrossRef - Management of Blood Pressure in Patients with Type 2 Diabetes Mellitus: A Nationwide Survey in Korean
Mi Hae Seo, Woo Je Lee, Cheol Young Park, Sung Rae Kim, Joong Yeol Park, Kun-Ho Yoon, Moon Kyu Lee, Sung Woo Park
Diabetes & Metabolism Journal.2011; 35(4): 348. CrossRef - Accuracy Evaluation of the Alternative Site Blood Glucose Test Using Error Grid
Kyung-Soon Park, Eun-Jong Cha
Journal of Biomedical Engineering Research.2011; 32(1): 25. CrossRef - Glycated albumin is a useful glycation index for monitoring fluctuating and poorly controlled type 2 diabetic patients
Eun Young Lee, Byung-Wan Lee, Daham Kim, Yong-ho Lee, Kwang Joon Kim, Eun Seok Kang, Bong-Soo Cha, Eun Jig Lee, Hyun Chul Lee
Acta Diabetologica.2011; 48(2): 167. CrossRef - Group Classification on Management Behavior of Diabetic Mellitus
Sung-Hong Kang, Soon-Ho Choi
Journal of the Korea Academia-Industrial cooperation Society.2011; 12(2): 765. CrossRef - Predictive Clinical Parameters for the Therapeutic Efficacy of Sitagliptin in Korean Type 2 Diabetes Mellitus
Soon Ae Kim, Woo Ho Shim, Eun Hae Lee, Young Mi Lee, Sun Hee Beom, Eun Sook Kim, Jeong Seon Yoo, Ji Sun Nam, Min Ho Cho, Jong Suk Park, Chul Woo Ahn, Kyung Rae Kim
Diabetes & Metabolism Journal.2011; 35(2): 159. CrossRef - Epidemiology of Micro- and Macrovascular Complications of Type 2 Diabetes in Korea
Jung Hee Kim, Dae Jung Kim, Hak Chul Jang, Sung Hee Choi
Diabetes & Metabolism Journal.2011; 35(6): 571. CrossRef - Increasing Trend in the Number of Severe Hypoglycemia Patients in Korea
Jin Taek Kim, Tae Jung Oh, Ye An Lee, Jun Ho Bae, Hyo Jeong Kim, Hye Seung Jung, Young Min Cho, Kyong Soo Park, Soo Lim, Hak Chul Jang, Hong Kyu Lee
Diabetes & Metabolism Journal.2011; 35(2): 166. CrossRef - Prevalence and Associated Factors of Diabetic Retinopathy in Rural Korea: The Chungju Metabolic Disease Cohort Study
Ji-Hyun Kim, Hyuk-Sang Kwon, Yong-Moon Park, Jin-Hee Lee, Man-Soo Kim, Kun-Ho Yoon, Won Chul Lee, Bong-Yun Cha, Ho-Young Son
Journal of Korean Medical Science.2011; 26(8): 1068. CrossRef - The Prevalence of Peripheral Arterial Disease in Korean Patients with Type 2 Diabetes Mellitus Attending a University Hospital
Ji Hee Yu, Jenie Yoonoo Hwang, Mi-Seon Shin, Chang Hee Jung, Eun Hee Kim, Sang Ah Lee, Eun Hee Koh, Woo Je Lee, Min-Seon Kim, Joong-Yeol Park, Ki-Up Lee
Diabetes & Metabolism Journal.2011; 35(5): 543. CrossRef - Prevalence, Awareness, and Control of Hypertension among Diabetic Koreans
Hyun Hee Chung, Kyu Chang Won
Diabetes & Metabolism Journal.2011; 35(4): 337. CrossRef - Factors Influencing Physical Activity Behavior among Iranian Women with Type 2 Diabetes Using the Extended Theory of Reasoned Action
Alireza Didarloo, Davoud Shojaeizadeh, Hassan Eftekhar Ardebili, Shamsaddin Niknami, Ebrahim Hajizadeh, Mohammad Alizadeh
Diabetes & Metabolism Journal.2011; 35(5): 513. CrossRef - Factors that Affect Medication Adherence in Elderly Patients with Diabetes Mellitus
Kyung-Ae Park, Jung-Guk Kim, Bo-Wan Kim, Sin Kam, Keon-Yeop Kim, Sung-Woo Ha, Sung-Taek Hyun
Korean Diabetes Journal.2010; 34(1): 55. CrossRef - The Effects of Tailored Diabetes Education on Blood Glucose Control and Self-Care
Kyung Sun Hyun, Kwang Mi Kim, Sook Hee Jang
Journal of Korean Academy of Nursing.2009; 39(5): 720. CrossRef - Epidemiologic Characteristics of Diabetes Mellitus in Korea: Current Status of Diabetic Patients Using Korean Health Insurance Database
Ie Byung Park, Sei Hyun Baik
Korean Diabetes Journal.2009; 33(5): 357. CrossRef
- Risk of Diabetic Complications in Type 2 Diabetes Patients with Dementia: A Population-Based Study Using National Health Insurance Claims Data
- Prevalence of the Metabolic Syndrome in Type 2 Diabetic Patients.
- Tae Ho Kim, Dae Jung Kim, Soo Lim, In Kyung Jeong, Hyun Shik Son, Choon Hee Chung, Gwanpyo Koh, Dae Ho Lee, Kyu Chang Won, Jeong Hyun Park, Tae Sun Park, Jihyun Ahn, Jaetaek Kim, Keun Gyu Park, Seung Hyun Ko, Yu Bae Ahn, Inkyu Lee
- Korean Diabetes J. 2009;33(1):40-47. Published online February 1, 2009
- DOI: https://doi.org/10.4093/kdj.2009.33.1.40
- 2,379 View
- 27 Download
- 13 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The aim of this study was to analyze the prevalence of metabolic syndrome in Korean type 2 diabetic patients. METHODS: A total of 4,240 diabetic patients (male 2,033, female 2,207; mean age 58.7 +/- 11.3 years; DM duration 8.9 +/- 7.6 years) were selected from the data of endocrine clinics of 13 university hospitals in 2006. Metabolic syndrome was defined using the criteria of the American Heart Association/National Heart Lung and Blood Institute and the criteria of waist circumference from the Korean Society for the Study of Obesity. RESULTS: The prevalence of metabolic syndrome was 77.9% (76.7% of males, 78.9% of females). The average number of the components of metabolic syndrome was 2.4 +/- 1.1. Abdominal obesity was seen in 56.8% of the patients, hypertriglyceridemia in 42.0%, low HDL cholesterol in 65.1%, and high blood pressure in 74.9%. Abdominal obesity and high blood pressure were much more prevalent among females than males, and low HDL cholesterol was much more prevalent among males than females. The prevalence of metabolic syndrome was not different according to the duration of diabetes. Metabolic syndrome was strongly related with obesity (odds ratio, 6.3) and increased age (odds ratio in the over 70 group, 3.4). CONCLUSION: The prevalence of metabolic syndrome was 77.9% in Korean type 2 diabetic patients. Its prevalence was greater in obese patients and in those over 40 years of age. -
Citations
Citations to this article as recorded by- A Novel Clinical Predictor of Metabolic Syndrome: Vascular Risk Age
Abdulrahman Naser, Didar Elif Akgün, Rengin Çetin Güvenç, Samet Sayılan, Özgen Şafak
Bagcilar Medical Bulletin.2023; 9(1): 1. CrossRef - Risk of Carotid Atherosclerosis in Subjects with Prediabetes Overlapping Metabolic Syndrome
Seol A Jang, Kyoung Min Kim, Seok Won Park, Chul Sik Kim
Metabolic Syndrome and Related Disorders.2022; 20(10): 599. CrossRef - Metabolic Age, an Index Based on Basal Metabolic Rate, Can Predict Individuals That are High Risk of Developing Metabolic Syndrome
Sarahi Vásquez-Alvarez, Sergio K. Bustamante-Villagomez, Gabriela Vazquez-Marroquin, Leonardo M. Porchia, Ricardo Pérez-Fuentes, Enrique Torres-Rasgado, Oscar Herrera-Fomperosa, Ivette Montes-Arana, M. Elba Gonzalez-Mejia
High Blood Pressure & Cardiovascular Prevention.2021; 28(3): 263. CrossRef - Metabolic syndrome among type 2 diabetic patients in Sub-Saharan African countries: A systematic review and meta-analysis
Wondimeneh Shibabaw Shiferaw, Tadesse Yirga Akalu, Mihretie Gedefaw, Denis Anthony, Ayelign Mengesha Kassie, Worku Misganaw Kebede, Henok Mulugeta, Getenet Dessie, Yared Asmare Aynalem
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2020; 14(5): 1403. CrossRef - Optimal Waist Circumference Cutoff Value Based on Insulin Resistance and Visceral Obesity in Koreans with Type 2 Diabetes
Jung Soo Lim, Young Ju Choi, Soo-Kyung Kim, Byoung Wook Huh, Eun Jig Lee, Kap Bum Huh
Diabetes & Metabolism Journal.2015; 39(3): 253. CrossRef - The Relations between Diabetic Dietary Compliance, Dietary Intake, and Physical Activity and the Prevalence of Metabolic Syndrome (MS) in Type 2 Diabetic Patients
Dong Eun Kim, Seung Hee Hong, Ji-Myung Kim
Korean Journal of Community Nutrition.2015; 20(5): 351. CrossRef - The Comparison between Periodontal Health Status and the Findings of Hypertension and Diabetes Disease of some Workers
In-Young Ku, Seon-Jeong Moon, Kyung-Hwan Ka, Myeong-Seon Lee
The Korean Journal of Health Service Management.2013; 7(2): 81. CrossRef - The Relationship between Factors of Metabolic Syndrome in Korean Adult Males and the Parents' Family History of Diabetes
Hyung-Su Park, Jin-Gyu Jeong, Jin-Ho Yu
The Journal of the Korea institute of electronic communication sciences.2013; 8(5): 779. CrossRef - Associations of serum fetuin-A levels with insulin resistance and vascular complications in patients with type 2 diabetes
Chan-Hee Jung, Bo-Yeon Kim, Chul-Hee Kim, Sung-Koo Kang, Sang-Hee Jung, Ji-Oh Mok
Diabetes and Vascular Disease Research.2013; 10(5): 459. CrossRef - Cardio-Metabolic Features of Type 2 Diabetes Subjects Discordant in the Diagnosis of Metabolic Syndrome
Sa Rah Lee, Ying Han, Ja Won Kim, Ja Young Park, Ji Min Kim, Sunghwan Suh, Mi-Kyoung Park, Hye-Jeong Lee, Duk Kyu Kim
Diabetes & Metabolism Journal.2012; 36(5): 357. CrossRef - Comorbidity Study on Type 2 Diabetes Mellitus Using Data Mining
Hye Soon Kim, A Mi Shin, Mi Kyung Kim, Yoon Nyun Kim
The Korean Journal of Internal Medicine.2012; 27(2): 197. CrossRef - Therapeutic Target Achievement in Type 2 Diabetic Patients after Hyperglycemia, Hypertension, Dyslipidemia Management
Ah Young Kang, Su Kyung Park, So Young Park, Hye Jeong Lee, Ying Han, Sa Ra Lee, Sung Hwan Suh, Duk Kyu Kim, Mi Kyoung Park
Diabetes & Metabolism Journal.2011; 35(3): 264. CrossRef - The Correlations between Extremity Circumferences with Total and Regional Amounts of Skeletal Muscle and Muscle Strength in Obese Women with Type 2 Diabetes
Hwi Ryun Kwon, Kyung Ah Han, Hee Jung Ahn, Jae Hyuk Lee, Gang Seo Park, Kyung Wan Min
Diabetes & Metabolism Journal.2011; 35(4): 374. CrossRef
- A Novel Clinical Predictor of Metabolic Syndrome: Vascular Risk Age
- Mechanism of 2-Deoxy-D-ribose-induced Damage in Pancreatic beta-cells.
- Gwanpyo Koh, Jeong taek Woo, Dae Ho Lee, Seungjoon Oh, Sung Woon Kim, Jin Woo Kim, Young Seol Kim, Deok Bae Park
- Korean Diabetes J. 2007;31(2):105-112. Published online March 1, 2007
- DOI: https://doi.org/10.4093/jkda.2007.31.2.105
- 2,060 View
- 21 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Mechanism for glucose toxicity is known to be an increased oxidative stress produced by multiple pathways. In our previous report, 2-deoxy-d-ribose (dRib) promoted apoptosis by increasing oxidative stress in a pancreatic beta-cell line. We performed this study to investigate the mechanism of dRib-induced damage of beta-cells. METHODS: HIT-T15 cells were cultured in RPMI-1640 medium with 40 mM dRib for 24 hours after pretreatment with various concentrations of a metal chelator (DTPA) and inhibitors of protein glycation (aminoguanidine and pyridoxamine). Cell viability was determined by MTT assay. Apoptosis was analyzed by flow cytometry with annexin V/PI double staining. RESULTS: DTPA, which inhibits the monosaccharide autoxidation, partially reversed dRib-induced cytotoxicity in a dose-dependent manner (P < 0.01). The cytotoxicity was also suppressed dose-dependently by aminoguanidine (AG) and pyridoxamine (PM) (P < 0.05 and P < 0.01, repectively). Flow cytometric analysis showed that pretreatment of DTPA and AG also reversed the dRib-triggered apoptosis in a dose-dependent manner. We assessed the additional protective effects of inhibitors of protein glycation from dRib-induced cytotoxiciy in the presence of a metal chelator. The additions of AG (P < 0.05) and PM (P < 0.01) significantly reduced the cytotoxicity compared with DTPA alone group. CONCLUSION: This results suggest that dRib produce cytotoxicity and apoptosis through the mechanisms of advanced glycation endproducts (AGEs) formation including the monsaccharide autoxidation and protein glycation in pancreatic beta-cell. Thus, dRib could be a surrogate for glucose in the study of glucose toxicity and chronic diabetic complications. -
Citations
Citations to this article as recorded by- Isolation of Citrus Peel Flavonoid Bioconversion Microorganism and Inhibitory Effect on the Oxidative Damage in Pancreatic Beta Cells
Chi-Deok Park, Hee-Kyung Jung, Chang-Ho Park, Yoo-Seok Jung, Joo-Heon Hong, Hee-Sun Ko, Dong-Hee Kang, Hyun-Soo Kim
KSBB Journal.2012; 27(1): 67. CrossRef - Kaempferol protects HIT‐T15 pancreatic beta cells from 2‐deoxy‐D‐ribose‐induced oxidative damage
Yun Jung Lee, Kwang Sik Suh, Moon Chan Choi, Suk Chon, Seungjoon Oh, Jeong‐Taek Woo, Sung‐Woon Kim, Jin‐Woo Kim, Young Seol Kim
Phytotherapy Research.2010; 24(3): 419. CrossRef
- Isolation of Citrus Peel Flavonoid Bioconversion Microorganism and Inhibitory Effect on the Oxidative Damage in Pancreatic Beta Cells
- Clinical Experience of the Reverse Iontopheresis Based Glucose Measuring System: GlucallTM.
- Sang Youl Rhee, Suk Chon, Gwanpyo Koh, Seungjoon Oh, Jeong Taek Woo, Sung Woon Kim, Jin Woo Kim, Young Seol Kim
- Korean Diabetes J. 2005;29(2):167-172. Published online March 1, 2005
- 918 View
- 16 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Finger pricking is currently the common method of blood glucose measurement in patients with diabetes mellitus. However, diabetes patients have proven reluctant to regularly check their glucose profiles because of the small amount of blood that is required. Recently, a non-invasive and continuous glucose monitoring device that is based on reverse iontophoresis(GlucallTM) has been developed. In this study we wanted to evaluate the accuracy and the clinical acceptability of this new device. METHODS: The study was conducted during the period from November 2003 to January 2004 on 19 in-patients who had been admitted to Kyung Hee University Hospital. Glucose measurements using GlucallTM were performed between 10am and 4pm. The concurrent plasma glucose levels were checked hourly and they were subsequently compared with the GlucallTM data. RESULTS: The mean error(ME) of the GlucallTM measurements was -3.45+/-52.99mg/dL with a mean absolute relative error(MARE) of 20+/-15.16%. Measurements obtained by GlucallTM had a correlation coefficient of 0.784(P<0.05) with the plasma glucose levels, as was determined by linear regression analysis. This correlation was consistent regardless of the time of data collection. However, after excluding such confounding variables as age and gender, the correlation coefficient exhibited a tendency to increase. 98.9% of the results were clinically acceptable according to Clarke error grid analysis. CONCLUSION: GlucallTM does not yet have the reliability and accuracy to wholly replace the conventional methods. However, further technical advancements to reduce its shortcomings will make this device useful for the management of diabetes patients
- A Case of Failure in Insulin Pump Treatment due to Abdominal Subcutaneous Fat Atrophy and Lipohypertrophied Nodules.
- Sang Youl Rhee, Suk Chon, Gwanpyo Koh, Seungjoon Oh, Jeong taek Woo, Sung Woon Kim, Jin Woo Kim, Young Seol Kim
- Korean Diabetes J. 2004;28(6):547-553. Published online December 1, 2004
- 954 View
- 20 Download
-
 Abstract
Abstract
 PDF
PDF - The insulin pump is an effective glycemic control device those function is analogous to the physiologic regulation of insulin in vivo. When sufficient patient education and proper selection of patients is done, the insulin pump is one of the most effective treatment modalities for diabetic patients. However, various side effects and complications might occur during its application. We report here on an unusual case of diabetic ketoacidosis that was caused by acute inflammatory colitis and insulin pump malfunction. Peculiarly, the cause of pump malfunction was far removed from its mechanical problem. We concluded that the cause of the insulin pump malfunction was due to abdominal subcutaneous fat atrophy and the lipohypertrophied nodules of the patient that developed due to the prolonged usage of the insulin pump.

 KDA
KDA
 First
First Prev
Prev





